Designing a full-system implantable neuromodulation device can be complicated regarding the engineering aspect, quality control, safety and reliability concerns. COFORCE Medical provides a thorough analysis of specifications, components, assembly and packing from the design and development point of view.
As we age, our brain and nerve system undergo many changes that can lead to neurology diseases. In the Rotterdam Study conducted by Rens Hanewinckel 2016, the prevalence of polyneuropathy, a condition in which a person's peripheral nerves are damaged, in the general middle-aged and elderly population is at least 4%, and increases with age from 2.4% of the group aged 50-60 years old to more than 12.6% of the group over 70 years old. Another current study published by Maeng Je Cho has reviewed epidemiological findings regarding geriatric mental health in Korea. Up to 10 % of the elderly aged 65 and over suffer from dementia, 33% from depression and 9% from Alzheimer's disease.
Poor medication compliance (like seizure medications), ineffectual existing treatments, the complexities of clinical practice and side effects have led to the fast growth of Neuromodulation as a life changing alternative for refractory patients.
Fig 1. Common neuromodulation indications.
Neuromodulation is technology that acts directly upon nerves. It alters - or modulates - nerve activity by delivering electrical or pharmaceutical agents directly to a target area. The use of neuromodulation devices and treatments to provide patients with continuous and stable symptom control has become a widely accepted treatment modality.
Since 2015, the U.S. Food and Drug Administration (FDA) has issued over 693 devices under its Breakthrough Devices Program. 126 of these breakthrough device designations are falling into the neurology field. Invasive neurology treatments in the current clinical practice include Deep Brain Stimulation (DBS) for Parkinson’s Disease, Cochlear Implants (CIs) as hearing aids, Vagus Nerve Stimulation for Epilepsy and Depression, and Spinal Cord Stimulator (SCS) for low back pain. These techniques have been proven to achieve good response rates for disease control.
In addition to the above neuromodulation technologies that have been approved by the FDA, there are a number of novel devices targeting different indications under development. For example, use DBS surgery in Stroke Rehabilitation, or treat Tourette’s Syndrome and Attention Deficit Hyperactivity Disorder (ADHD). Other applications focusing on organ functions regulation, such as treatment of eating disorders by Gastric (GI) Stimulation, are also being seen.
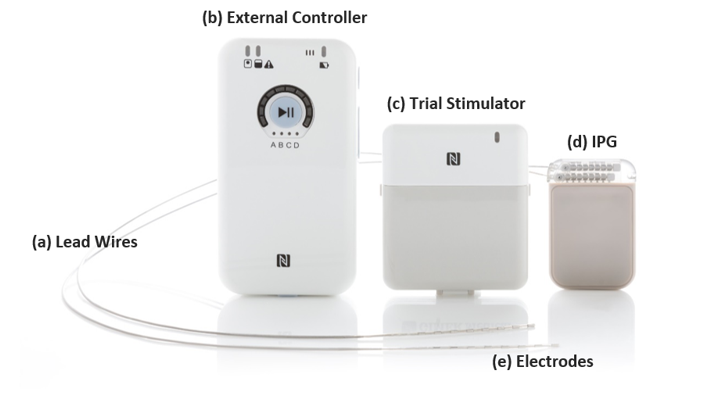
Fig 2. Full-system device analysis: from the designing view.
Most neurostimulators conform to a similar design: an implanted part and a PC-based external controller that allows the patient as well as clinician to adjust the therapy. There are three primary components in the implanted part, which are - An Implantable Pulse Generator or neurostimulator, to generate the electrical currents - Single or multiple leads to transmit the current from IPG to the target site, and - An array of electrodes located in close proximity to the nervous tissue applies voltage pulses.
Depending on the clinical scenarios, some systems may be designed with an additional stimulator trial. The trial is intended to closely resemble the results of the actual procedure, except that the device transmitting current is not implanted in the body, but the lead wires are inserted and sends electrical signals to the certain nerve via an external transmitter. The trial phase typically takes around two weeks to test the patient’s response rate to the treatment and make sure if it is something that will help them long-term. If the patient achieves a certain level of symptom improvement at the end of the trial phase, the patient may proceed with full system implantation. Otherwise the implant can be removed or reprogrammed with minimized damage to the target nerve or brain tissue.
Fig 3. Different types of electrodes for neuromodulation.
Commonly used electrodes in neuromodulation include those shown in figure above. The form selection and the implantation method depend on the target disease and neural tissue. For instance, since a DBS stimulator discharges electrical current within the globus pallidus internal segment (GPi) or the subthalamic nucleus (STN), the percutaneous lead, shaped like a wire, is then often chosen for this kind of device. Opposed to the percutaneous lead, the paddle shaped electrode is used in devices like permanent SCS. This kind of electrodes lay closer to the spinal cord due to the dimensions and surgical placement of the paddle form. It allows for increased stimulation while avoiding painful stimulation, enhancing the likelihood of capturing elusive back pain.
Other common electrodes can be named a few: neural cuff electrodes, stereoelectroencephalography (SEEG) electrodes. The former leaves room for nerve swelling immediately after implantation while still maintaining a snug fit for good electrical contact, and for preventing movement-induced injury; while the later uses deep electrodes to record brainwaves (EEG) from inside the head temporarily which allows the identification of epileptogenic zones for tailored resection surgery in epilepsy patients.
In the development process of an implanted neuromodulation device, the stimulator is the most challenging in terms of reliability, safety, integration and optimization. The role of the implantable neurostimulator includes the complex interconnection of connectors, implanted lead and electrodes, steady output of electrical stimulation signals, continuous monitoring of the system operation to ensure its safety, and reliable wireless communication with external controllers. The design of such a device that is interacting with all elements of the whole stimulation system requires a highly multidisciplinary approach which involves disciplines such as neuroscience, electrophysiology, electrochemistry and electrical engineering.
First and foremost, the team of design and development needs to carry out the work in order to build a reliable multi-application stimulation system, from integrated circuit design to user interface. Second but not less important, they should use proper hermetic sealing techniques to package and prevent the system from failures caused by body fluid leakage. Moreover, it is the designers’ responsibility to always integrate proactive safety by medical device risk analysis and management in their design. The devices mentioned above are expected to be implanted in the patient’s body for a long-term period of more than five or even ten years.
How to ensure operational safety? How to select suitable materials that are functionality compliance and biocompatibility? And how to implement design controls, risk management process, document and records maintenance as well as supplier management throughout the product life cycle?
Fig 4. COFORCE Medical – Asia’s pioneer outsourcer.
By following a structured, methodical approach with traceability throughout, device makers may massively improve the success rate of clinical approval and accelerate time to market of their products. The biggest problem is - where should you start with?
COFORCE Medical Inc. is Asia’s pioneer medical device outsourcer. We have more than 10 years of expertise in design and developing implantable bioelectronics. Backed up by a large pool of selective technical partners and high-quality components supplies from Taiwan, we have integrated a reliable, affordable med-tech supply chain to fulfill our clients' needs.
We can provide services including but not limited to rapid modular R&D, FDA communication consulting, 3rd party laboratories collaboration, and batch / mass production in strictly controlled environment. With our tailored targeted solutions for your device, you can rely on us as a collective force. From feasibility evaluation, design and development throughout long-term manufacturing and assembly, we can help you shorten your development cycle , prepare your design controls for regulatory approval and finally bring your med-tech innovation to life within time and budget.
Fig 4. COFORCE Medical – Asia’s pioneer outsourcer.
By following a structured, methodical approach with traceability throughout, device makers may massively improve the success rate of clinical approval and accelerate time to market of their products. The biggest problem is - where should you start with?
COFORCE Medical Inc. is Asia’s pioneer medical device outsourcer. We have more than 10 years of expertise in design and developing implantable bioelectronics. Backed up by a large pool of selective technical partners and high-quality components supplies from Taiwan, we have integrated a reliable, affordable med-tech supply chain to fulfill our clients' needs.
We can provide services including but not limited to rapid modular R&D, FDA communication consulting, 3rd party laboratories collaboration, and batch / mass production in strictly controlled environment. With our tailored targeted solutions for your device, you can rely on us as a collective force. From feasibility evaluation, design and development throughout long-term manufacturing and assembly, we can help you shorten your development cycle , prepare your design controls for regulatory approval and finally bring your med-tech innovation to life within time and budget.